By Ross Pelton, Scientific Director, Essential Formulas
Help Protect Yourself Against C. diff Infections
With Dr. Ohhira’s Probiotics®
Every cold and flu season, there is an enormous surge in the number of antibiotic prescriptions dispensed in pharmacies, urgent care clinics, and hospitals. Unfortunately, this phenomenon seems to be contributing to the global problem of antibiotic-resistant “superbugs.” And one of the worst of these superbugs is Clostridium difficile.
C. difficile spores have a hard, outer coat that allows them to survive the harsh, acidic environment of the human stomach. After they arrive in the large intestine/colon area of the GI tract, they germinate, which means that they cease being dormant spores and begin to grow and become active. This is when they start to produce and secrete their toxins.
Clostridium difficile (frequently referred to as C. diff) is a pathogenic strain of bacteria that is becoming an increasingly serious health threat. C. diff produces toxins that are extremely irritating to cells in the intestinal tract, which frequently causes intense inflammation and severe diarrhea in afflicted people. The United States is currently experiencing an accelerating epidemic of toxic and often deadly Clostridium difficile infections.
Currently, there are about 500,000 cases of CDIs reported in the United States each year, and the latest statistics indicate that about 29,000 people die from CDIs annually. In fact, most people don’t realize that more people in the United States are currently dying from C. diff infections than from HIV and AIDS combined.
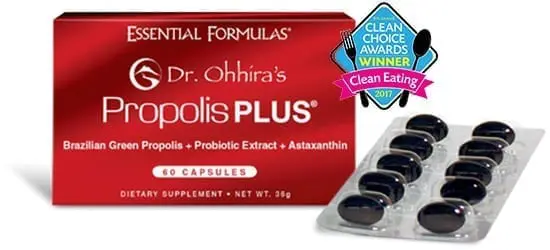
Numerous studies and scientific experts agree that maintaining a healthy microbiome is the primary key for protecting oneself against C. diff infections.i I recommend Dr. Ohhira’s Probiotics® to help people do this. Other steps to support a healthy immune system include taking vitamin D, vitamin C and omega-3 fish oil supplements, as well as eating a balanced diet, engaging in regular exercise, and getting adequate sleep.
History of Clostridium difficile Infections
C. difficile infections have historically been seen primarily as a hospital-acquired infectious disease problem, and C. diff is currently the leading cause of hospital-acquired illness in the United States. However, there is also an alarming increase in the number of Clostridium difficile infections (CDIs) in non-hospitalized patients. For example, in one study, 41% of CDIs were community-acquired rather than hospital-acquired.ii
C. difficile spores have a hard, outer coat that allows them to survive the harsh, acidic environment of the human stomach. After they arrive in the large intestine/colon area of the GI tract, they germinate, which means that they cease being dormant spores and begin to grow and become active. This is when they start to produce and secrete their toxins.
We are in the midst of a C. diff infection epidemic. Currently, there are about 500,000 cases of CDIs reported in the United States each year, and the latest statistics indicate that about 29,000 people die from CDIs annually. In fact, most people don’t realize that more people in the United States are currently dying from C. diff infections than from HIV and AIDS combined.
Asymptomatic Clostridium difficile
Many people carry C. diff bacteria in their GI tract but do not manifest symptoms of a CDI. This is called asymptomatic Clostridium difficile
Some studies suggest that approximately 15% of healthy adults harbor C. diff. In hospitalized elderly patients, asymptomatic C. diff may be present in up to 51% of the population. And among healthy newborn infants, the prevalence of asymptomatic C. difficile has been reported to be as high as 90%.
I believe that far more people in the general population have C. diff bacteria in their GI tract than the figures in the previous paragraph indicate. In fact, I wouldn’t be surprised if we someday learn that most people have C. diff. However, in many individuals, a few C. diff bacteria do not create problems. This is because, traditionally, small numbers of C. diff do not lead to infections.
Clostridium difficile Infections Are Increasing
The primary cause for the alarming upswing in the incidence of C. diff infections is due to the widespread use—and over-use—of antibiotics. Problems of this nature manifest in three ways:
- C. difficile is naturally opportunistic. Taking oral antibiotics to prevent or treat infection often has the negative side effect of destroying your system’s beneficial bacteria. This weakens your microbiome overall. And in a distressed microbiome, C. diff bacteria can flourish.
- C. difficile is becoming antibiotic-resistant: When C. diff bacteria are exposed to an antibiotic, some of the C. diff develop immunity or resistance to that particular antibiotic. Then, the next time you get sick and receive another round of antibiotics, some C. diff bacteria are immune, and even more C. diff bacteria become resistant.
- C. difficile is becoming more toxic: Bacteria are incredibly productive. In addition to antibiotic resistance, newer, hyper-virulent strains of C. diff are reportedly secreting from 16 to 23 time more toxins than previous strains, and the newer toxins have a much higher level of potency.iii
Numerous studies and scientific experts agree that maintaining a healthy microbiome is the primary key for protecting oneself against C. diff infections.i I recommend Dr. Ohhira’s Probiotics® to help people do this. Other steps to support a healthy immune system include taking vitamin D, vitamin C and omega-3 fish oil supplements, as well as eating a balanced diet, engaging in regular exercise, and getting adequate sleep.
Postbiotic Metabolites
Dr. Ohhira’s Probiotics® are an excellent choice to keep your gut bacteria strong and robust because they are fermented food products that deliver postbiotic metabolites in every single dose. Various postbiotic metabolites are key essential nutrients, while others provide anti-inflammatory activity, antibiotic activity against pathogens, anti-yeast and anti-fungal activity, and some even improve detoxification and help maintain the optimal acid/base balance in your GI tract.
Postbiotic metabolites play critical roles in the maintenance of a healthy microbiome. This is the Dr. Ohhira’s Difference!™
i Schubert AM, et al. Microbiome Data Distinguish Patient with Clostridium difficile Infection and Non-C. difficile-Associated Diarrhea from Healthy Controls. mBio. 2014;5(3):e01021-14.
ii Khanna S, et al. The Epidemiology of Community-acquired Clostridium difficile infection: A population-based study. Am J Gastroenterol. 2012 Jan; 107(1):89-95.
iii Warmy M., et al. Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet. 2005 Sep 24-30;366(9491):1079-84.