By Ross Pelton, RPh, PhD, CCN
An alarming study from Washington University St Louis (WUSTL) recently reported that antibiotic resistant “superbug” infections are killing more than 153,000 annually in the United States. This figure is nearly seven times greater than the CDC’s previous estimate of 23,000 deaths per year.
To put this crisis in perspective, let’s look at cancer deaths. The National Cancer Institute (NIH) estimates that in 2018, about 41,000 women will die from breast canceri and about 30,000 men will die from prostate cancerii, which totals 71,000. This means that antibiotic resistant ‘Superbug’ infections are killing two times more Americans than the combined number of men and women dying from prostate and breast cancers!
The Gut Immune System
The lining of your intestinal tract is the largest surface area of your body that is exposed to the environment. In fact, the surface area of the human gastrointestinal track is from 15 to 20 times greater than the surface area of your skin.iii The lining of the intestinal tract, which is referred to as the gut immune system contains 70-80% of the body’s immune cells. Thus, keeping your gut/microbiome healthy is the key to keeping your immune system healthy,
Numerous factors can influence the immune system such as zinc, vitamin D levels, stress and exposure to environmental toxins to name a few. Unfortunately, most people don’t understand the critical importance of the gut immune system and how to keep it functioning at a high level of efficiency.
How to Create and Maintain a Healthy Gut Immune System
The following three components are necessary to create and maintain a healthy gut immune system.
- A healthy population (85-90%) of friendly probiotic bacteria
- Regular ingestion of fiber-rich foods, which “feed” your probiotics
- Postbiotic metabolites; health-regulating compounds produced by probiotic bacteria when they digest/ferment fiber-rich foods
The FIBER Gap: An article titled The Fiber Gap and the Disappearing Gut Microbiome: Implications for Human Nutrition discusses how low fiber diets are affecting people’s microbiome and ultimately, their health. The authors of this study report that an alarming 90% of children and adults in America DO NOT consume the recommended amount of daily dietary fiber.iv
Probiotic bacteria digest/ferment dietary fibers to produce a wide range of compounds called postbiotic metabolites. Just as the computers at NASA’s mission control center regulate space flights, postbiotic metabolites are the “mission control” compounds that help regulate the function of every organ system in the body, especially the immune system and the brain.
Because dietary fiber is so deficient in the Standard American Diet (SAD), many people probably get very little benefit from the probiotics they take. A diversity of dietary fibers is critical for a healthy microbiome. A lack of dietary fiber has three potentially serious consequences.
- Your probiotic bacteria will not be able to produce the important health-regulating postbiotic metabolites.
- Your probiotic bacteria will die off (starve) because you are not providing them with dietary fibers which are their required foods.
- Bad bacteria will proliferate due to decreasing numbers of probiotic bacteria and the reduction or absence of postbiotic metabolites.
Each of these three consequences of a low fiber diet can cause or contribute to a wide variety of health issues ranging from intestinal problems to autoimmune diseases.
Antibiotic Resistant ‘Superbug’ Infections
The overprescribing of antibiotics is one of the most serious causes of the dramatic increase in Superbug infections. The amount of inappropriate prescribing of antibiotics by physicians is staggering. For example, acute bronchitis is a respiratory illness that usually resolves in less than 3 weeks without treatment. Over the past 40 years, multiple clinical trials have shown that antibiotics are not effective for acute bronchitis.v However, a recent study published in the Journal of the American Medical Association (JAMA) reported that doctors prescribed antibiotics for over 70% of bronchitis cases.vi In another study the CDC reported that about 1/3 of antibiotic prescriptions prescribed in outpatient settings are unnecessary.vii
Another aspect of the problem is that many people ask for or demand an antibiotic prescription every time they get a cold, the flu or their child gets the first sign of an earache. Part of the reason physicians over prescribe antibiotics is that they respond to the expectations of their patients.
Physicians also express concerns about getting poor patient satisfaction ratings when they decline a patient’s request for an antibiotic. In one survey, 59% of physicians reported that their compensation was linked to patient satisfaction ratings, 20% said their employment was threatened due to low patient satisfaction ratings and 50% said pressure to gain better patient ratings contributed to prescribing unnecessary antibiotics.viii
‘Superbug’ infections are caused by strains of pathological bacteria that have developed resistance to virtually all antibiotics. Organizations such as the US Centers for Disease Control and Prevention (CDC), the European Centre for Disease Prevention and Control (ECDC) and the World Health Organization (WHO) agree that the rapid rise of antibiotic resistant bacterial infections is a critical global health crisis.ix The World Health Organization is also projecting that if this trend continues, by 2050 these infections will kill over ten million people each year.x
Many Americans believe we have the most advanced health care system in the world. However, a recent survey reported that of the 206 countries in the world, the United States has the third highest occurrence of antibiotic resistant bacterial infections (China and Kuwait are first and second).xi
The situation is so critical that many healthcare professionals are calling it a “nightmare scenario” that could have catastrophic consequences for the human race.xii Also, in 2013, the World Health Organization (WHO) declared that the human race is already in the “post-antibiotic era,” meaning we are at a point where antibiotics will continue to be less and less effective, and eventually will not be effective at all. The seriousness of this trend is staggering.
The use of antibiotics in the industry of raising food animals such as cows, chickens and pigs is also a major contributor to the development of antibiotic-resistant bacteria. The living conditions for animals raised for food in “factory farming” operations are notoriously inhumane. The stress and depression in animals raised under these conditions results in weakened immune systems which increases their susceptibility to infectious diseases. Consequently, animals are prophylactically treated with antibiotics in an effort to prevent diseases.xiii Antibiotics are also widely used to promote weight gain.xiv
Conclusion
Efforts to reduce physician overprescribing of antibiotics and to reduce or eliminate the regular use of antibiotics in agricultural animals are important goals. However, the most important aspect of reducing the incidence of antibiotic resistant Superbug infections is to teach people how to create and maintain a healthy microbiome which is the foundation of a heathy immune system.
In a recent program titled Healing from GMOs and Roundup, host Jeffrey Smith interviewed Zach Buch, MD. In that interview, Dr. Bush made the following comment, which I tend to agree with:
“There is no such thing as bad bacteria. There is just bad balance.”
If people maintain a healthy microbiome with 85-90% beneficial probiotic bacteria AND they regularly ingest a wide range of diverse fiber-rich foods, then their probiotic bacteria will constantly produce a wide range of postbiotic metabolites that regulate their immune system and their health.
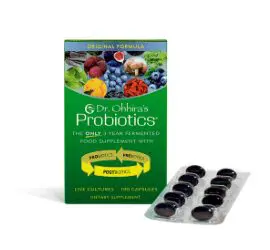
At Essential Formulas, we firmly believe that Dr. Ohhira’s Probiotics are the best product available to help people maintain a heathy microbiome because it delivers a complete microbiome system consisting of probiotic bacteria, prebiotic foods and over 400 postbiotic metabolites.
As far as we know, Dr. Ohhira’s Probiotics is the only product in the world that utilized a multi-year fermentation production process that allows the probiotic bacteria time to ferment the fiber-rich foods they are supplied with, which results in the production of over 400 postbiotic metabolites. By directly delivering postbiotic metabolites, Dr. Ohhira’s Probiotics rapidly initiates improvements in people with a wide range of gastrointestinal problems.
That’s The Dr. Ohhira’s Difference
Dr. Ohhira’s Probiotics are available at most vitamin and health food stores and online at Amazon.com.