Original Post Date:
June 25, 2021
Dysbiosis, (which is also called dysbacteriosis), is a term that indicates an imbalance of bacteria in or on the body. While dysbiosis most commonly refers to a microbial imbalance in the intestinal (GI) tract, it can also denote an imbalance of bacteria on the skin, known as skin dysbiosis.
The gut microbiome is frequently altered in people with skin conditions.iii Studies have confirmed that skin dysbiosis is present in skin irregularities such as atopic dermatitis, psoriasis, rosacea, acne vulgaris, eczema, and dandruff.iv
This is hardly surprising considering the numerous similarities the gut and skin share. Both act as a barrier between harmful pathogens and the body’s immune system, and when either is compromised—such as when dysbiosis occurs—it can have significant ramifications for your overall health. Since everything in the body is ultimately connected, if something happens in the gut, it can eventually affect your skin, and manifest as one of the abovementioned skin conditions.
For instance, if the gut’s microbiome is compromised in such a way that it allows pathogens to pass through the intestinal wall, it can lead to an immune response throughout the body, including at skin level. This in turn may affect the skin’s microbiome as well. Since your diet is a major factor that regulates the bacterial composition in your gut microbiome, your skin health can be impacted significantly by what you eat. Likewise, research suggests that it’s possible to mitigate skin conditions by working from the inside out.
Shocking Frequency of Skin Complaints
A large study conducted by the Mayo Clinic between 2005 and 2009 revealed that skin concerns are the most common reasons people visit their doctor.v According to the Mayo Clinic study, 43% of patients made a doctor’s appointment for a skin disorder compared to 33.6% for joint conditions, 23.9% for back problems, 22.4% for cholesterol problems.
Cancer is still the #1 killer in the U.S., nearly half of Americans have high blood pressure, and over one-third of Americans have diabetes or prediabetes. Thus, it was surprising to learn that skin disorders are responsible for more doctor visits than these more common high-profile diseases. The realization that skin diseases are associated with skin dysbiosis emphasizes the importance of maintaining a healthy skin microbiome.
Balance
Most of the bacteria in the gut and on the skin of healthy individuals are beneficial. Balance is the key to both a healthy gut microbiome and a healthy skin microbiome. The gut and skin of all people contain some potentially harmful bacteria. Still, when your microbiomes are predominantly populated with beneficial bacteria, the harmful bacteria cannot multiply and cause problems. Thus, it is essential to realize that skin dysbiosis, like gut dysbiosis, is primarily a microbiome problem being out of balance.
Skin Postbiotic Metabolites
In 2019, an article titled Postbiotic Metabolites: The New Frontier in Microbiome Science explained that probiotic bacteria in the GI tract produce health-regulating compounds we refer to as postbiotic metabolites.vi We are now learning that beneficial bacteria that live on your skin also produce important health-regulating postbiotic metabolites.
Healthy skin is slightly acidic, which results from the bacteria in the skin microbiome producing postbiotic metabolites that are weakly acidic compounds.
Another important class of skin postbiotic metabolites is called antimicrobial peptides (AMPs). AMPs are natural antibiotics that are produced by various strains of probiotic bacteria, both in the gut and on the skin. AMPs are an important part of our immune system because they kill and/or inhibit the growth of pathogens. Many strains of beneficial skin bacteria make various antimicrobial peptides, which suppress the growth of pathogens and accelerate wound healing.vii
Staphylococcus aureus is a strain of bacteria associated with numerous skin diseases such as eczema, atopic dermatitis, psoriasis, and a high level of S. aureus is an indicator of skin dysbiosis. A healthy skin microbiome contains strains of bacteria that produce AMPs which suppress the growth of S. aureus.viii
A species of skin bacteria named Propionibacterium produces an antimicrobial peptide called Enterocin AS-48. It has been shown to have significant antibacterial activity against 23 different bacteria strains commonly associated with acne.ix
Staphylococcus epidermidis is a beneficial strain of skin bacteria found to produce a postbiotic metabolite named butyric acid. Butyric acid functions is multiple ways to promote a healthy microbiome in the gut and on the skin.x
In a survey of bacteria isolated from seven body sites, researchers were able to identify 21 different previously unknown postbiotic antimicrobial peptides that exhibited activity against a wide range of skin pathogens.xi
The growing understanding that different species of beneficial skin bacteria produce and secrete postbiotic metabolites that help to maintain a healthy skin microbiome is an exciting new area of science.
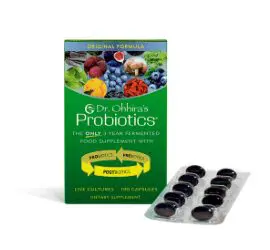
The first record of topical probiotic therapy occurred in the Journal of Cutaneous Diseases in 1912, which reported the topical application of Lactobacillus bulgaricus to treat acne.xii However, it took nearly 100 years before dermatologists understood how beneficial topical probiotics could be to treat skin irregularities. In 2014, the American Academy of Dermatologists issued a statement calling probiotics a “Beauty Breakthrough.”
Topical probiotics can improve the quality and health of your skin by supplying healthy bacteria to your skin’s microbiome. The postbiotic metabolites produced by the probiotic bacteria help suppress harmful strains, resulting in improved dermic health. Of course, the right formulation of probiotics and ingredients will provide the best results.
Vitamin D and Gut Health
Just as dermic health can be affected by the types of bacteria in your gut, so too could your gut’s health be impacted by your skin. During the summer months, for instance, UV rays can have a dramatic effect on the skin by triggering vitamin D production. Vitamin D has been shown to promote intestinal health, and a vitamin D deficiency could lead to gut dysbiosis, as demonstrated in a recent study in Frontiers in Microbiology. In this study, researchers found that increased exposure to UVB rays had similar effects on microbiome diversity as taking vitamin D supplements.
FAQs on the Gut-Skin Connection
Do probiotics help with skin health?
Probiotics can help support skin health, due to the postbiotic metabolites they create. .
Is gut health related to acne? Can probiotics help with acne?
Gut health and acne have been shown to be related. Many studies have indicated that there may be a connection between the bacterial composition in the gut and the prevalence of acne, with acne patients exhibiting a decrease in probiotic species (such as Lactobacillus and Bifidobacterium) that normally help balance the gut microbiome and strengthen the intestinal barrier. As such, probiotics can be useful to support healthy skin tissue.
Can gut health affect the skin?
As demonstrated by the numerous studies already cited here, your gut and skin microbiomes work together to build the integrity of your skin.
How to Protect Your Skin Microbiome
Here is a list of critical factors that are important for creating and maintaining a healthy skin microbiome:
- Eat a healthy diet: avoid processed foods, minimize sugar, consume a high quantity and diversity of fiber-rich foods.
- An allergy or sensitivity to food(s) or environmental agents (soap, detergent, household cleaning agent, cosmetics) can cause itchy, painful skin conditions to develop.
- Get adequate omega-3 fatty acids in the diet or as nutritional supplements. Omega-3 oils support health in numerous ways. They are important regulators of skin health and the immune system.xiii
- Protect skin from excessive exposure to UV light.
- Maintain a healthy gut microbiome. Studies have reported a strong link between microbiome imbalances in the gut and various skin conditions.xiv
- Read the book Clean: The New Science of Skin by James Hamblin, MD. Dr. Hamblin suggests stopping or dramatically reducing the use of strong chemically based shampoos, conditioners, and cleaners, which tend to damage the skin microbiome. Select natural products that promote skin integrity and a healthy skin microbiome.
To learn more about ways to protect and balance your skin’s microbiome, go to www.EssentialFormulas.com
References:
i Arck P, et al. Is there a ‘gut-brain-skin axis’? Exp Dermatol. 2010 May;19(5):401-405.
ii Salem I, et al. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front Microbiol. 2018;9:1459.
iii Szanto M, et al. Targeting the gut-skin axis—Probiotics as new tools for skin disorder management? Exp Dermatol. 2019 Nov;28(11):1210-1218.
iv De Pessemier B, et al. Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms 2021 Feb 11; 9(2):353.
v St. Sauver JL, et al. Why Patients Visit Their Doctors: Assessing the Most Prevalent Conditions in a Defined American Population. Mayo Clinic Proceedings. Jan 1, 2013;88(1):56-67.
vi Pelton R. Postbiotic Metabolites: The New Frontier in Microbiome Science. Townsend Letter. 2019 June;431:61-69.
vii Grice EA and Segre JA. The Skin Microbiome. Nature Reviews Microbiology. 2011 Apr;9(4):244-53.
viii Ryu S, et al. Colonization and Infection of the Skin by S. aureus: Immune System Evasion and the Response to Cationic Antimicrobial Peptides. Int J Mol Sci. 2014;15(5):8753-8772.
ix Cebrian R, et al. The potential of bacteriocin AS-48 in the control of Propionibacterium acnes. Scientific Reports. 2018 Aug 6;8(11766.
x Keshari S. et al. Butyric Acid from Probiotic Staphylococcus epidermidis in the Skin Microbiome Down-Regulates the Ultraviolet-Induced Pro-Inflammatory IL-6 Cytokine via Short-Chain Fatty Acid Receptor. Int J Mol Sci. 2019 Sep 11;20(18):4477.
xi O’Sullivan JN, et al. Human skin microbiota is a rich source of bacteriocin-producing staphylococci that kill human pathogens. FEMS Microbiology Ecology. Feb 2019;95(2):fiy241.
xii Peyri J: Topical bacteriotherapy of the skin. J Cutaneous Dis. 1912, 30: 688-89.
xiii Balic A, et al. Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases. Int J Mol Sci. 2020 Jan 23;21(3):741.
xiv Szanto M, et al. Targeting the gut-skin axis-Probiotics as new tools for skin disorder management? Exp Dermatol. 2019 Nov;28(11):1210-1218.