By Ross Pelton, RPh, PhD, CCN
Scientific Director, Essential Formulas
The gut microbiome is increasingly being recognized as a key factor in the aging process. This has raised the question, which is a better predictor of your long-term health and your risk of developing age-related diseases, your genes or microbiome? This article will review the exciting results from two large studies that address this issue.
The Human Genome Project revealed that humans contain approximately 2,000 genes. Subsequently, results from the Human Microbiome Project reported that around 1,000 different species of bacteria reside in and on humans, which collectively contain about 3.3 million unique genes. Consequently, the human microbiome is frequently referred to as our “second genome.”
The enormous predominance of microbial genes compared to the number of our human genes has stimulated research to discover which genome, human or bacterial, has the most significant influence on health and longevity. The results may surprise you.
STUDY #1: Taxonomic Signatures of Long-Term Mortality Risk in Human Gut Microbiota.
In 1972, the Health Department in Finland began collecting data on thousands of people utilizing surveys and health exams to assess lifestyle factors and the risk for chronic diseases. The surveys and health exams were repeated every five years for 40 years, from 1972 to 2012.i
In 2002, the subjects also donated stool samples sequenced 15 years later. Scientists analyzed the microbiome from the stool samples of 35,499 participants and compared it with their human genome/DNA. They also analyzed blood samples from 21,087 participants between the ages of 25 and 74.
This study is now referred to as the FINRISK Study.ii The quantity and the quality of the data collected, the number of people involved, and the length of time of the study make the FINRISK Study one of the most important health studies ever conducted. More than 1,100 articles or reports and 65 doctoral dissertations have been published based on the results from the FINRISK Study.
STUDY #1 RESULTS:
Individuals whose microbiome contained more significant numbers of bacteria classified as pathogens such as Salmonella, E. coli, Klebsiella, Shigella, Proteus, and Citrobacter were 15% more likely to die within the next 15 years. The risk of dying was similar for people living in different geographical regions in Finland and among people with different lifestyles and genetics. Thus, an individual’s microbiome was more accurate than the human genome at predicting an individual’s long-term risk of dying.
STUDY #2: The predictive power of the microbiome exceeds that of genome-wide association studies in the discrimination of complex human diseases.iii
This paper is a meta-analysis of 47 different studies that evaluated the predictive capabilities of an individual’s human genome versus their microbiome for 13 common diseases. The assessed diseases include the following: asthma, colon cancer, high blood pressure, obesity, Parkinson’s disease, prostate cancer, rheumatoid arthritis, schizophrenia, type 1 diabetes, type 2 diabetes, ulcerative colitis, and Crohn’s disease.
STUDY #2 RESULTS:
Overall, the results revealed that an analysis of the structure, function, and diversity of an individual’s microbiome was approximately 20% more accurate at predicting the incidence of the diseases studied than an analysis of the individual’s human genome/DNA. Analysis of the human microbiome was 50% more accurate in predicting colon cancer. Human DNA was only better at predicting type 1 diabetes of the diseases studied.
My Comments & Analysis
These studies support the hypothesis that maintaining a healthy microbiome is critical for good health. In fact, the results from these studies suggest that maintaining a healthy gut microbiome maybe is a more important determinant of your health than your genes. Yet, there are many things in today’s world that harm or destroy the microbiome, far too many to list here. However, I want to discuss one of the most critical issues that determines your microbiome’s health, which is bacterial diversity.
The Importance of a Diverse Microbiome
Throughout nature, the health of ecosystems depends on biodiversity. In coral reefs, the Amazon rainforest, and your gut microbiome, greater diversity results in better health, strength, and resilience. But, what is the meaning of diversity? In various ecosystems, greater diversity means more species of animals, plants, trees, insects, birds, etc. In your gut microbiome, greater diversity means a broader range of different species of probiotic bacteria.
You cannot increase your microbiome diversity by just taking probiotics. The only way to create greater microbiome diversity is by consuming a greater variety of plant-based foods. Different species of bacteria require different kinds of food. The two primary types of food probiotic bacteria require are dietary fibers and polyphenols. The richest source of these probiotic-friendly foods are colored vegetables and fruits, followed by grains, nuts, seeds, herbs, and spices, and let’s not forget chocolate.
Postbiotic Metabolites
When probiotic bacteria are provided with a diverse range of polyphenols and dietary fibers, they convert these non-digestible dietary components into postbiotic metabolites. It is becoming increasingly clear that postbiotic metabolites are critical health-regulating compounds for the body. Although they are produced in the colon, they influence every organ system in the body, including the brain and the immune system.
The Malnourished Microbiome
For 99.9% of human evolution, people consumed foods that grew naturally in nature. Unfortunately, most people today consume enormous amounts of canned, packaged, and highly processed foods, which are severely deficient in the types of compounds that probiotic bacteria require to thrive and produce postbiotic metabolites. Scientists estimate that our ancient ancestors consumed from 5 to 10 times more dietary fibers and polyphenols than modern humans. The dramatic decline in the consumption of plant-based foods results in a malnourished microbiome. This, in turn, allows the proliferation of harmful bacteria, which creates a dysfunctional microbiome ecosystem. This often results in damage to the lining of the intestinal tract, which can lead to a wide range of more severe health problems. Most diseases begin in the gut.
The Postbiotic Solution
In a healthy microbiome, probiotic bacteria produce many different types of postbiotic metabolites. Some of their essential functions include suppressing the growth or directly killing pathogens, creating the optimal level of acidity, reducing and/or repairing damage to the gut lining, and stabilizing and enhancing the immune system. Postbiotic metabolites are key regulators of your health.
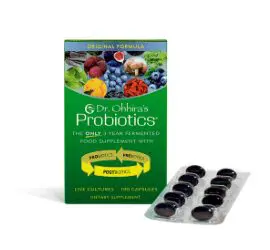
Dr. Ohhira’s Probiotics
In addition to switching to a plant-based diet, one of the most effective ways to help correct a dysfunctional microbiome ecosystem is to consume postbiotic metabolites directly. The best way to accomplish this is by taking Dr. Ohhira’s Probiotics, which are produced in a multi-year fermentation process that results in the creation of over 500 postbiotic metabolites. The postbiotic metabolites in Dr. Ohhira’s Probiotics accelerate the re-establishment of a healthy microbiome ecosystem, which often quickly resolves gastrointestinal problems. This is why Dr. Ohhira’s Probiotics has gained a worldwide reputation for providing fast relief from dysbiosis-related gastrointestinal symptoms.