Scientific Director, Essential Formulas
Dysbiosis is a condition that is caused by a bacterial imbalance in the gastrointestinal tract, which frequently causes symptoms such gas, bloating, inflammation, pain and diarrhea or constipation.
I’m proposing the existence of a condition I’m naming Asymptomatic Dysbiosis, which refers to a low level of dysbiosis that does not cause overt symptoms, yet it causes chronic inflammation that is associated with a wide range of health problems and accelerated biological aging.
A review of the intestinal microbiome and the consequences of bacterial imbalance in the gastrointestinal tract provide a foundation for a discussion of asymptomatic dysbiosis.
Understanding the Microbiome
The intestinal microbiome refers to the organisms that reside in the gastrointestinal tract such as bacteria, fungi, viruses, and archaea. In this article, when I use the term microbiome, I will only be referring to the bacteria in the intestinal tract.
The intestinal microbiome is estimated to contain approximately 100 trillion bacteria consisting of 500 to 1,000 different species of bacteria.i However, the gut microbiome in each individual is estimated to contain about 160 different species of bacteria.
A healthy microbiome is estimated to have approximately 85-90% good bacteria (probiotics) and only 10-15% bacteria that are potential pathogens.ii When good bacteria predominate, small numbers of “bad” bacteria do not cause problems. Potential pathogens only cause problems when they are allowed to proliferate, which results in microbial imbalance or dysbiosis.iii Over 99% of the bacteria in the human gastrointestinal tract reside in the colon, which is an anaerobic environment. Hence, when dysbiosis occurs, it is usually due to bacterial imbalance in the colon.iv
Causes of Dysbiosis:
Many diet, lifestyle, and environmental factors can cause or contribute to intestinal bacterial imbalance. Major disruptive factors include processed foods, which lack fiber, high intake of dietary sugar and fatv, antibiotics, using acid-suppressing drugsvi, excess alcohol consumptionvii, sleep disorders such as insomnia and sleep apneaviii, to name a few. Because so many microbiome-disrupting factors are common in today’s world, many people suffer from dysbiosis.
I intend to show that many people unknowingly suffer from asymptomatic dysbiosis. Even though there are no symptoms, asymptomatic dysbiosis has been shown to cause chronic inflammation, which accelerates biological aging.
Zonulin & Tight Junctions
Alessio Fasano, MD is Professor of Pediatrics at Harvard Medical School. His brilliant research resulted the discovery of zonulin, which is a protein that is expressed in response to inflammation. When zonulin levels are elevated, it degrades the proteins that are the basis of tight junctions between epithelial cells in the gastrointestinal tract.
Tight junctions are critical for the integrity of the barrier that constitutes the lining of the GI tract. Tight junctions are formed by proteins on the surface of the epithelial cells that line the gastrointestinal tract. Metaphorically, tight junction proteins function somewhat like Velcro, which holds neighboring cells tightly together.
When dysbiosis occurs, the elevated number of “bad” bacteria cause inflammation in the lining of the intestinal tract. This results in an increased production of zonulin, which results in the breakdown of the tight junctions. Damage to tight junctions allows harmful substances from the intestinal tract, such bacteria, viruses and partially digested food particles to “pass through the intestinal barrier and enter into systemic circulation. This condition is called intestinal permeability or “leaky gut”. When intestinal permeability occurs, one of the most damaging substances that can pass into systemic circulation is are compounds knows as lipopolysaccharides or LPS.
Lipopolysaccharides (LPS)
Lipopolysaccharides (LPS) are part of the cell membrane of many types of bacteria in the intestinal tract. Everyone has LPS in their intestinal tract, but they are supposed to stay in the intestinal tract and be eliminated via bowel movements. When LPS leak through damaged tight junctions and enter systemic circulation, they are highly toxic substances that cause inflammation throughout the body.
Chronic low levels of circulating LPS are associated with the development of some of our most common diseases such as type 2 diabetes, atherosclerosis, heart diseases and obesity.ix,x LPS are especially toxic to neurons and are associated with neurodegenerative diseases such as cognitive decline and age-related neurodegenerative disorders.xi
Asymptomatic Dysbiosis
Many people unknowingly suffer from asymptomatic or sub-clinical dysbiosis. This condition allows small amounts of LPS to pass through damaged tight junctions and enter systemic circulation. The level of LPS may be so low it doesn’t cause any overt symptoms. However, small amounts of LPS have been shown to cause chronic inflammation throughout the body. Chronic inflammation, which is now referred to as “inflamm-aging” is strongly implicated in age-related diseases and the acceleration of biological aging.xii
Landmark Study: Injecting low dose LPS
In a double-blind, placebo-controlled, crossover study, healthy, young volunteers were randomly divided into two groups (A & B). Patients were housed in an inpatient clinical facility and intravenously administered either a low dose of LPS or saline and given a standardized diet for two separate 36-hour inpatient visits.
PART 1: Group A was administered a low dose of LPS intravenously and Group B was administered IV saline as the placebo. Following the IVs, patients filled out a symptom & pain questionnaire at 1, 2, 4, 6, 12, 18 and 24 hours. Blood was drawn to evaluate a wide range of markers, and several other tests were performed.
Part 2: After a one-month washout period, the groups were reversed. This time Group B received the IV LPS and Group A was administered IV saline placebo.
RESULTS: The amount of LPS that was administered intravenously was so low, none of the participants experienced any symptoms; no one was aware of receiving a dose of LPS. However, when scientists conducting the study evaluated the blood samples, they discovered that low-dose LPS IV caused a 25-fold increase in plasma levels of tumor necrosis factor alpha (TNF-alpha) and a 100-fold increase in plasma levels of interleukin-6 (IL-6).xiii Both TNF-alpha and IL-6 are well documented markers of inflammation that are associated with accelerated biological aging.xiv,xv
Even though there were no symptoms, a low level of LPS entering circulation causes significant chronic inflammation throughout the body, which is associated with biological aging.xvi,xvii
The Microbiome Diet
If you don’t feed your probiotic bacteria well, they will not thrive and survive. The two types ‘foods’ that probiotic bacteria require are dietary fibers and polyphenols.xviii,xix Humans do not possess the enzymes required to metabolize most dietary fibers. Hence, dietary fibers travel through the GI track unchanged until they reach the colon, where they are fermented by probiotic bacteria and converted into metabolites with a wide range of biological activity. Some species of probiotic bacteria possess many different enzymes that enable them to metabolize dozens of different types of dietary fibers, while others are only able to utilize one or a few types of fiber.xx
Many polyphenols are very large, complex molecules, which humans also do not digest well. Consequently, they remain unabsorbed in the small intestines, but when they reach the colon, they undergo fermentation by probiotic bacteria and get converted into metabolites with a wide range of biological activity. Plant-based foods (vegetables and fruits) contain the highest quantity of dietary fibers and polyphenols. Smaller amounts are in herbs, spices, nuts, olives, coffee, and tea.
Postbiotic Metabolites
The primary “job” of probiotic bacteria is to convert dietary fibers and polyphenols into smaller compounds that have a wide range of biological activity. Postbiotic metabolites are now being recognized as the new frontier in microbiome science.xxi In addition to regulating the health of the gastrointestinal ecosystem, many postbiotic metabolites get absorbed into systemic circulation, which enables them to influence and help regulate other systems including the brain, lung, heart, liver, heart, skin and immune system.xxii
Function of Postbiotic Metabolites
In The Mind-Gut Connection, Emeran Mayer, MD states, “Your bacteria use the information stored in their millions of genes to transform food into hundreds of thousands of metabolites.”xxiii If Mayer is right, and I believe he is, then postbiotic metabolites are the new frontier in microbiome science. We are just beginning to learn about the multitude of postbiotic metabolites that probiotic bacteria can make, which species most effectively make various postbiotic metabolites, what their functions are, and what types of dietary fibers and/or polyphenols enable the bacteria to make different kinds of postbiotic metabolites.
Some of the important functions of postbiotic metabolites include:
- Antioxidant activity: Lactobacillus fermentum ME-3 is a strain of bacteria that directly synthesizes glutathione.xxiv Other strains of probiotic bacteria can produce important antioxidant enzymes such as catalase, superoxide dismutase and glutathione peroxidase.xxv
- Anti-inflammatory activity: Metabolites of many strains of probiotic bacteria exhibit anti-inflammatory activity.xxvi,xxvii
- Antimicrobial peptides (AMPs): AMPs can directly kill and/or suppress the growth of pathogensxxviii,xxix Pathogens do not develop resistance to AMPs; AMPs can kill antibiotic-resistant bacteria such as MRSA.xxx
- Regulate acidity: Many postbiotic metabolites are weakly acidic compounds, which play key roles in regulating the level of acidity in the GI tract. In addition to short-chain fatty acids (SCFAs), which include acetic, propionic and butyric acids, other weakly acidic postbiotic metabolites include organic acids, nucleic acids, amino acids and fulvic acids.xxxi Taking antibiotics orally destroys the probiotic bacteria that normally produce acidic postbiotic metabolites. This dramatically increases alkalinity in colon.xxxii The resulting alkaline environment is favorable for the subsequent proliferation of pathogens.
- Enhance Immune Function: Postbiotics can enhance immunity by improving intestinal barrier function, which inhibits ability of LPS and pathogens from entering systemic circulation. Postbiotic metabolites also regulate innate and adaptive immune function by interacting with B cells, T cells, NK cells, monocytes, macrophages, and dendritic cells along the lining of the intestinal tract.xxxiii
The Malnourished Microbiome
Multiple studies have reported that most American children and adults (from 80-95%) do not consume adequate amounts of dietary fibers and polyphenols.xxxiv,xxxv,xxxvi,xxxvii This means their intestinal bacteria are not capable of making adequate amounts of postbiotic metabolites, which results in dysbiosis, inflammation, intestinal permeability, and accelerated biological aging.
The Diversity Dilemma
In virtually all ecosystems, greater diversity results in greater strength and resilience. This is especially true for the human intestinal microbiome. However, different species of bacteria require different types of food. This is why it is so important for people to consume a diverse range of plant-based foods every day. People should strive to eat a small amount of many different types of plant-based foods every day. This will provide a diverse range of dietary fibers and polyphenols, which will support the growth of a diverse range of probiotic bacteria, so that they can produce a diverse range of health-regulating postbiotic metabolites.
The ONLY way individuals can create and maintain a microbiome with a high level of diversity is by consuming a diet that contains a diversity of dietary fibers and polyphenols, which will promote the growth and proliferation of many different species of probiotic bacteria, and the production of a diverse range of postbiotic metabolites.
The Oral Probiotic Dilemma
The oral probiotic industry in the United States was estimated to be $17.4 billion in 2022. Unfortunately, most of these products are not providing the benefits people think they are. Here’s why.
Problem #1: Gastric acidity is the first part of the oral probiotic dilemma. Stomach acid is designed to kill; it is from 10,000 to 100,000 times stronger than the acidity in the rest of the intestinal tract. Most orally ingested probiotics are killed when they are exposed to stomach acid. Enteric coated probiotics and spore-based probiotics are exceptions to this rule; they can survive transit through the stomach. However, they are also likely to be ineffective, for reasons explained below.
Problem #2: The small intestine is also a very hostile environment for orally ingested probiotic bacteria. Intestinal fluids, especially bile acids and pancreatic enzymes, have antimicrobial activity, which reduces the viability and survival of orally ingested probiotic bacteria in the small intestine.xxxviii
Problem #3: The third dilemma is the fact that most people do not consume an adequate quantity or diversity of dietary fibers and polyphenols. Thus, even if orally ingested probiotics successfully transit through the stomach and small intestines, when they arrive in the colon, they will not be able to produce sufficient postbiotic metabolites to insure good health.
Who Suffers from Asymptomatic Dysbiosis?
I think most people alive today suffer from asymptomatic dysbiosis and the resulting chronic inflammation is playing a major role in the declining health of humanity. Here is the evidence to support my hypothesis.
The health of humanity has rapidly declined over the past century. In the United States in the early 1900s, the three leading causes of death were pneumonia, tuberculosis, and diarrhea, which was caused by intestinal infections. In the 1950s and 1960s, America did not have epidemics of age-related diseases.
Currently in the US, and increasingly in other countries, we are experiencing an epidemic of epidemics; (heart disease, cancer, diabetes, inflammatory bowel diseases, obesity, autism, Alzheimer’s disease, etc.). To drive home the point, in 2019, the American Heart Association reported that nearly 50% of Americans have heart disease.xxxix Over two-thirds (69%) of U.S. adults are overweight or obese.xl Nearly 38 million Americans (11.3%) have diabetes.xli Over 20% of Americans live with mental illness.xlii And then, we had a 3-year (March 2020-May 2023) COVID-19 pandemic. And now we have long COVID.
And then there’s our children. Over 50% of American children has one or more of the following diseases: food allergies, endocrine disorders, obesity, autoimmune diseases and/or neurocognitive disorders. It is frightening to realize that over half of American children currently have a potentially life-long disease.xliii Sadly, for the first time ever, children living today are expected to have a shorter life expectancy than their parents.xliv
How Did We Get Here?
American Health Care Is Broken was the title of an article in the May 2023 issue of Time magazine.xlv The U.S. spends over $4 trillion (20% of our gross domestic product) a year on health care. Nearly all the money spent on health care goes to pay for medical treatments. Unfortunately, the American Health Care system is failing miserably in the prevention and treatment of chronic degenerative diseases.
Rather than spending trillions of dollars trying to treat individual diseases, it would make much more sense to try and prevent or correct an underlying problem that is related to all age-related diseases, which is the dysregulated or unbalanced gastrointestinal microbiome. Support for the idea that the gut microbiome should be a major focus in the American medical and healthcare system comes from several well-respected sources.
In 2016, Cleveland Clinic, which is ranked as one of the top hospitals in the United States, convened a large panel of leading physicians and scientists to create a list of medical innovations with the greatest potential to transform healthcare in the future. After evaluating over 500 new therapies and medical innovations, the experts narrowed the list down to the top 10 medical innovations most likely to be “game changers” in healthcare and medicine.
The Top 10 Medical Innovations were announced to over 1,600 physicians, entrepreneurs, and industry leaders attending Cleveland Clinic’s 2017 Medical Innovation Summit. The big news at the Summit was:
Using the Microbiome to Prevent, Diagnose & Treat Disease.xlvi
A paper published in The Journal of Immunology reported that the lack of postbiotic metabolites is a key factor in the rapid rise in age related diseases. In their conclusion, the authors stated the following: “It is now clear that the depletion of microbial metabolites beneficial to host health is associated with a rapid rise in non-communicable chronic diseases (NCCDs).”xlvii
The two main disruptors of the gastrointestinal microbiome are antibiotics and the standard American diet (SAD). Antibiotics save lives. However, disturbing consequences of antibiotic therapy include long-term disruption of the gut microbiome and the development of antibiotic resistant such as MRSA and antibiotic resistant clostridium difficile.xlviii
The standard American diet is the biggest and most widespread cause of bacterial imbalance in the gastrointestinal tract. Homo sapiens have been evolving on earth for about 300,000 years and for over 99.9% of this time, humans consumed primarily a plant-based diet.
A recent survey announced that 73% of the U.S. food supply consists of ultra-processed foods.xlix Also, there are over 200,000 fast food restaurants in the US, (average of over 4,000/state).l These figures support the studies previously mentioned, which report that from 80-95% of Americans do not consume adequate amounts of food containing dietary fibers and polyphenols.
The lack of these dietary components results in the following cascade of events. Most people will not be capable of maintaining a diverse population of colonic probiotic bacteria; this results in dysbiosis and intestinal inflammation, elevated levels of zonulin and damage to intestinal tight junctions, which allows LPS to pass into systemic circulation.
The LPS study reviewed earlier in this paper documents that low levels of LPS may not cause noticeable symptoms, but it causes substantial chronic inflammation. The information about the sad state of food quality and the fact that most Americans consume a diet that does not promote a healthy microbiome supports the hypothesis put forth in this paper, that most people suffer from asymptomatic dysbiosis.
Asymptomatic Dysbiosis
Healthcare is a $2.5 trillion/year industry, which makes it one of the largest industries in the United States. However, much of this is not healthcare, it is disease care. Chronic disease accounts for 7 of every 10 deaths in the United States and more than 75% of total health care costs.li
Hippocrates is called the Father of Medicine, and he is credited with saying, “All Disease Begins in the Gut.” That statement is not totally correct. However, emerging evidence suggests that many of the most common chronic, age-related degenerative diseases are associated with dysbiosis, compromised gut barrier function, and systemic inflammation. Unfortunately, most people don’t realize that diabetes, heart disease, cancer, obesity and many other degenerative diseases are associated with intestinal dysbiosis. Addressing the epidemic of asymptomatic dysbiosis needs to become a priority in America. We need to educate people about how to create and maintain a healthy intestinal microbiome.
The Microbiome Diet: Every time you eat, you are feeding 100 trillion guests. The microbiome diet is a diet that supplies a diverse range foods that contain dietary fibers and polyphenols. I encourage people to watch my 8-minute YouTube video, which teaches people how easy It is to make a microbiome-supporting salad (and it is a big time-saver). Just to a Google search for: YouTube Ross Salad Buzz.
Dietary change is the most important action that needs to happen. People need to stop consuming high sugar and high fat meals and highly processed foods. Switching to a diet that contains a diversity of plant-based foods that contains a diversity of dietary fibers and polyphenols is essential.
Busting the Myth: It is important for people to realize that orally ingested high-dose probiotics don’t work very well. Taking 100s of billions of one or several strains of probiotic bacteria works against microbiome balance and diversity.
One study reported that ingesting high doses of Lactobacillus acidophilus triggered the immune system to mount an alarm reaction. In their conclusions, the authors stated: “Probiotics can be ineffective or even detrimental if not used at the optimal dosage for the appropriate purposes.”lii
In The Gut-Immune Connection, Emeran Mayer, MD states, “Taking the popular and highly advertised short cut of popping a daily supplement pill containing billions of colony-forming units (CFUs) will NOT do the job.”
Postbiotic Metabolites: The New Frontier in Microbiome Science
For a long time, people have intuitively believed that probiotic bacteria provided health benefits, but no one understood the mechanism of action. However, in my June 2019 article titled Postbiotic Metabolites: The New Frontier in Microbiome Science, I explained that the “job” of probiotic bacteria is to breakdown components in food, which results in the production of compounds with a wide range of biological activity.liii The process of bacterial breakdown is called fermentation, and the resulting byproducts are called postbiotic metabolites.
Oral Postbiotic Metabolites:
Postbiotics metabolites can be taken orally; they, are not destroyed by stomach acid and when they arrive in the colon, they immediately begin to exert beneficial changes. Taking postbiotic metabolites orally quickly induces positive changes in the intestinal microbiome ecosystem.
Some of the most important health benefits that postbiotic metabolites immediately begin to express include anti-inflammatory activity, directly killing or suppressing the growth of pathogens, restoring optimal level of acidity, reestablishing gut-brain communication, repairing the intestinal lining and reducing intestinal permeability, and improving immune function.
The Dr. Ohhira Story
Dr. Iichiroh Ohhira (1936-2016) was a visionary microbiologist whose career had a transformative impact on our understanding of how the intestinal microbiome regulates human health.
When Ohhira was a young man, he became a Buddhist monk. In his 30s, Ohhira enrolled in Okayama University and in 1973, he graduated with a master’s degree from the school of agriculture. After graduating, Ohhira started what became a very successful career as a landscape architect.
In 1976, Malaysia invited Ohhira to design a large ‘Freedom Park’ for the city of Kota Kinabalu, which is the capital of the Malaysian state of Sabah on the island of Borneo. Ohhira accepted this contract and in 1980, he was invited back to Malaysia to attend the grand opening ceremony at the park he had designed.
While attending the grand opening, Ohhira ate some tainted food that resulted in severe nausea and vomiting. A local shaman who was attending the ceremony saw Ohhira lying on the ground in obvious distress. He knelt and cradled Ohhira’s head in his lap and then he pulled a bottle from his leather bag and began spoon-feeding Ohhira a dark colored syrup-like substance. Ohhira was astounded at how quickly his nausea and vomiting abated.
Ohhira learned that the “miracle paste” was created from locally fermented Malaysian fruits and vegetables. He took some samples back to Japan, but he was unable to learn much about it because he didn’t have the necessary knowledge or training. Consequently, in 1987, at the age of 49, Ohhira abandoned his successful career as a landscape architect and enrolled in Okayama University’s graduate program in microbiology. Throughout his graduate program, he focused his research on Lactic Acid bacteria and the process of fermentation.
Dr. Ohhira graduated in 1990 with his Ph.D. in microbiology and this was the beginning of his remarkable second career. He spent the next ten years experimenting and ultimately, developing his multi-year fermentation process used to produce Dr. Ohhira’s Probiotics.
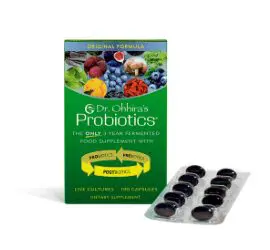
Dr. Ohhira’s Probiotics
Dr. Ohhira’s Probiotics are produced in 80-gallon fermentation vats in a sterile manufacturing facility in southern Japan. Dozens of healthfully grown Japanese fruits, vegetables, mushrooms, and seaweeds are added to the fermentation vats along with 12 strains of probiotic bacteria that Ohhira selected for their unique biological activity.
Dr. Ohhira’s Probiotics Original Formula is a 3-year fermentation process. Dr. Ohhira’s Probiotics Professional Formula gets an additional 2 years of anaerobic fermentation. During the multi-year production processes, the starter strains of bacteria ferment compounds in the foods (dietary fibers and polyphenols) and convert them into smaller compounds called postbiotic metabolites that have a wide range of biological activity. Each dose of Dr. Ohhira’s Probiotics contains over 500 postbiotic metabolites.
Mimicking Nature
Dr. Ohhira’s fermentation process mimics the natural fermentation processes that take place in the human colon. It takes food about 6-8 hours to pass through the stomach and small intestine. When ingested food enters the large intestine, it takes from 24-72 hours (average 36 hours) to travel through the entire colon. This is when trillions of bacteria ferment dietary fibers and polyphenols to produce critically important health-regulating postbiotic metabolites.
In humans, colonic bacteria have from 24-72 hours to ferment dietary fibers and polyphenols and produce postbiotic metabolites. But, most people do not consume an adequate quantity or diversity of plant-based foods. Hence, they are not able to produce adequate amounts of postbiotic metabolites, which results in either overt or asymptomatic dysbiosis.
Over 500 Postbiotic Metabolites
During the 3-year fermentation process for Dr. Ohhira’s Probiotics Original Formula, bacteria have 26,280 hours to ferment the prebiotic foods they are supplied with. The bacteria in Dr. Ohhira’s Probiotics Professional Formula have a total of 43,800 hours of fermentation time. Dr. Ohhira’s multi-year fermentation process results in the production of over 500 postbiotic metabolites.
Microbiome Insurance
Most people have medical insurance. Dr. Ohhira’s Probiotics, which contains over 500 postbiotic metabolites, is microbiome health insurance. The gut microbiome is a key regulator of health and microbiome dysfunction lies at the core of many chronic, age-related diseases.
Creating and maintaining a healthy gut microbiome is essential for good health and maintaining a healthy gut microbiome is the best health insurance against asymptomatic dysbiosis.
A healthy diet is essential for a healthy gut microbiome. However, in our modern world, most people do not consume a wide diversity of plant-based foods every day. Contrast this with Dr. Ohhira fermentation system in which bacteria are supplied with many types of fruits, vegetables, mushrooms, and seaweeds, and have thousands of hours to ferment these foods, and create over 500 postbiotic metabolites.
That’s the Dr. Ohhira’s Difference, that’s the Dr. Ohhira’s Advantage.