The Essential Guide to Taking Probiotics with Antibiotics
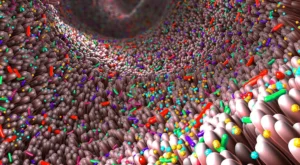
Antibiotics can be a lifesaving therapy for bacterial infections, but they come at a price. When they kill the “bad” bacteria, they also kill the “good” bacteria. They can change the intestinal environment – called the microbiome – reducing the diversity of friendly bacteria in the gut. This change can disrupt the body’s bacterial balance, negatively affecting the gut and overall health.
Researchers are debating whether the intestinal changes are temporary or permanent, but they have determined that antibiotic use leads to dysbiosis or a gut imbalance in the intestinal microbiome. In particular, they have noted a reduction in probiotics such as Lactobacillus and an increase in unfriendly bacteria. Each year, these harmful bacteria cause thousands of infections.
When the friendly bacteria disappear, the gut has space for unfriendly bacteria to take root and grow. Not only do these pathogenic bacteria cause damage to the microbiome and many systems in the body, but scientists also believe they are a factor in antibiotic-resistant infections.
Why is it Important to Take Probiotics with Antibiotics?
An imbalance in the gut microbiome often produces unpleasant symptoms and can lead to more serious problems. A probiotic supplement, that contains a variety of strains of beneficial microorganisms, can help to restore balance to the intestinal microbiome that may be disrupted by antibiotic use.
A Short Primer on Probiotics
Our bodies have an invisible internal life that goes on 24/7. Our skin, urogenital systems, mouths, and digestive systems host multitudes of microorganisms. Some are helpful, and some are detrimental to health.
Healthy people have a great diversity of healthy and unhealthy organisms in their bodies, starting at birth – about 300-1,000 different species. The microbiome matures to a nearly adult level around age two. When the bacteria are balanced, the friendly microorganisms predominate and do their business, positively affecting the body. But when something like antibiotic treatment disrupts the microbiome, trouble can start.
Prebiotics
Prebiotics are foods that promote or “feed” the probiotics or friendly bacteria in your body. They are composed of foods that contain undigestible fiber. When you eat certain undigestible foods, the fiber passes to the intestines, becoming nutrition for the probiotics.
Prebiotic foods contain “resistant starches,” and probiotics feed on these. Adding resistant starches to your diet gives the friendly bacteria the food they need to colonize and produce positive results. Add boiled, chilled potatoes, green-skinned bananas, barley, oats, rice, beans, and legumes to your diet to increase these resistant starches.
Postbiotics
Postbiotics are the outcome of the interaction between probiotics and prebiotics. They are the reason we take probiotics in the first place. Postbiotics are vitamins, amino acids, short-chain fatty acids, and enzymes. They are the natural products of a healthy microbiome and are also available in some supplements.
What Happens to the Gut with Antibiotic Use?
Your gut is healthiest when it contains a variety of probiotic species, each contributing something different to the body. These friendly bacteria boost our immune system and keep the pathogenic bacteria in check, among other positive effects.
Scientists are investigating probiotics’ effects on the heart, allergies, mood, and more. When antibiotics kill friendly and unfriendly bacteria, diversity decreases, leaving the body vulnerable to the unfriendly bacteria around us and ultimately impacting multiple body systems.
Antibiotic overuse creates a condition called antimicrobial resistance. Antimicrobial resistance is when the germs “learn” to overcome the drugs we usually use to kill them. To combat this, the CDC recommends asking your healthcare provider if you or your child really need antibiotics. Colds, and flu are viral infections, and antibiotics are ineffective against them.
What Is the Research on Taking Probiotics with Antibiotics?
If you’ve taken antibiotics, you are likely familiar with some of their uncomfortable gastric side effects. You’re not alone; 5-29% of people who take antibiotics experience them, and they can last for days or months. Some studies indicate that certain probiotics – friendly bacteria – can help bring the gut back into balance.
In a survey of 33 studies with children, participants received probiotics to take with an antibiotic. The authors concluded that probiotics improved gut issues in those who took them. Some sources say that pairing probiotics with antibiotics makes the antibiotics more effective and that, in some cases, antibiotics may not even be needed.
While researchers say that more in-depth studies are needed to identify which probiotics are best for different conditions, study results have been promising.
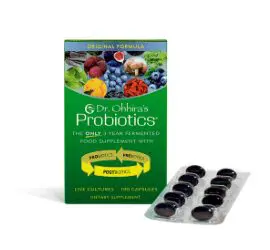
The Best Probiotics for Antibiotics
Which probiotic strains are best to take with antibiotics? The strains most tested were combinations of the following bacteria: Lactobacilli spp., Bifidobacterium spp., Streptococcus spp., and a probiotic yeast, Saccharomyces boulardii. Further, the incidence of adverse effects with these strains was very low.
Can Everyone Take Probiotics?
While probiotics are generally considered safe, those with immune system issues, recent surgery, or critical illnesses should consult their health professional before taking probiotics.
When Is the Best Time to Take Probiotics during Antibiotic Therapy?
There are no firm guidelines for when to take probiotics, but since antibiotics can kill the probiotics you take, experts suggest staggering ingestion. For instance, if you take the antibiotic in the morning, wait until evening to take your probiotic. Other healthcare providers recommend taking the probiotic 1-2 hours after taking your antibiotic.
Yeasts such as S. boulardii are probiotics, not bacteria, so antibiotics do not affect them.
How Long Should I Take Probiotics After Antibiotics?
Experts say that when you take probiotics with antibiotics, you should continue taking the probiotic up to two to four weeks after you finish your course of antibiotics. You can also help improve your microbiome by adjusting your diet to include more legumes, fruit, vegetables, whole grains, nuts, and seeds. Fermented foods are also helpful. Foods like yogurt, kefir, tofu, sauerkraut, miso, and kimchi contain probiotics, although you may not know what strains you are consuming or in what amounts.
Your gut health regimen doesn’t need to stop two weeks after antibiotic treatment. This modern world constantly bombards our bodies with stress, toxins, pollution, chemicals, and refined foods, which can negatively affect the microbiome. It is a smart practice to reinforce a healthy microbiome by taking a quality probiotic every day.