Heart disease is the leading cause of death among people in the U.S., so maintaining your cardiovascular health is definitely something to be thinking about. There are many ways to keep your heart healthy, and one of them appears to be related to your gut. A growing body of research shows that probiotics may help improve heart health.
The Heart-Gut Connection
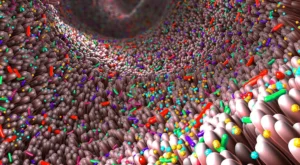
The organisms living in your gut can have a significant impact on many aspects of your health, including cardiovascular health. These organisms, referred to collectively as the microbiome, process what you eat into various chemicals. These chemicals are called postbiotic metabolites.
Some postbiotics can affect your cardiovascular health, such as by regulating blood pressure and cholesterol. Some research even suggests that having the right microbial balance in your gut may help with recovery after a heart attack.
Introducing the right bacteria—called probiotics—into your gut may be a way to improve heart health. Dietary matters can also play a role here. For instance, fiber—a prebiotic—can encourage the production of metabolites that regulate blood pressure. Red meat and eggs, on the other hand, may instead produce chemicals that promote arterial clogging, so it’s still important to watch what you eat.
Potential Impact of Probiotics on Heart Health
There’s a steadily growing body of data that indicates that certain probiotics may have a positive impact on heart health. There are a few ways in which this can occur, including the following.
Blood Pressure
Various studies indicate a relationship between your gut’s microbiome and blood pressure. A 2014 review of controlled trials showed that introducing multiple species of probiotics significantly reduced blood pressure, especially when used over a sustained period (8 weeks or more). Results were most pronounced when blood pressure was particularly high to begin with.
A review conducted in 2020 found similar results, with studies showing a “statistically significant” reduction of either systolic blood pressure or diastolic blood pressure in hypertension patients.
Growing evidence explains how the human gut microbiome regulates various aspects of human health that extend far beyond the gastrointestinal tract. The purpose of this article is to review studies that report that gut microbiome dysbiosis is strongly associated with high blood pressure.
Many genetic, environmental, diet, and lifestyle factors are associated with hypertension. However, the involvement of the gut microbiome is one factor that has been largely ignored and underestimated.
Previously, animal studies have reported an association between dysregulation of the gut microbiome and elevated blood pressure.i More recently, human clinical trials are reporting a clear relationship between an imbalance of the gut microbiome and high blood pressure. One of the primary findings is that intestinal barrier dysfunction, which is also called intestinal permeability, or “leaky gut,” is linked to elevated blood pressure in humans.ii
The CARDIA Study:
The CARDIA study (Coronary Artery Risk Development in Young Adults) began in 1985 with 5,115 participants. The CARDIA microbiome study is a 30-year follow-up examination designed to assess the relationship between the gut microbiome and blood pressure.iii
During the 30-year follow-up, researchers collected stool samples from 600 of the original participants and correlated their colonic microbiome with blood pressure.
The study revealed that having certain types of bacteria present in the colon is strongly associated with increased blood pressure.
A recent study published in the British Medical Journal reported that lifestyle changes might be more important than drugs to treat mildly elevated blood pressure.iv The authors of this study emphasized that you cannot cure high blood pressure by taking prescription drugs. Drugs only help to control high blood pressure as long as the individual continues to take them. You can only cure high blood pressure by changing the lifestyle factors that cause it.
Numerous diet and lifestyle factors influence blood pressure. The CARDIA study results suggest that diet and lifestyle changes can help lower elevated blood pressure because they increase the quantity and diversity of probiotic bacteria and the production of healthful postbiotic metabolites such as the short-chain fatty acid butyrate.
At Essential Formulas, we suggest that the most vital method to create and maintain an optimally healthy microbiome is to consume a diet containing a wide variety of fiber-rich food along with taking two capsules of Dr. Ohhira’s Probiotics daily.
Dr. Ohhira’s probiotics are produced in a multi-year fermentation process, which results in a final product that contains probiotics, prebiotics, and over 500 postbiotic metabolites. The direct delivery of a wide range of postbiotic metabolites explains why Dr. Ohhira’s Probiotics frequently elicit rapid improvement of gastrointestinal symptoms such as gas, bloating, diarrhea, and inflammation. This is referred to as The Dr. Ohhira’s Advantage!
Cholesterol
Cholesterol is another component of cardiovascular health that may be positively impacted by probiotics. A review of 32 randomized controlled trials showed that there was a significant reduction of total cholesterol when probiotic supplements were used.
In addition, one meta-analysis found that certain strains of the probiotic Lactobacillus were particularly effective at reducing total cholesterol and LDL cholesterol. At the same time, there was also some indication that HDL cholesterol (the good kind) could be benefitted by eating foods with a mix of probiotics and prebiotics (called synbiotics).
-
 Dr. Ohhira’s Probiotics®$13.95 – $89.95Price range: $13.95 through $89.95
Dr. Ohhira’s Probiotics®$13.95 – $89.95Price range: $13.95 through $89.95 -
 Dr. Ohhira’s® Probiotics Professional Formula$39.95 – $129.65Price range: $39.95 through $129.65
Dr. Ohhira’s® Probiotics Professional Formula$39.95 – $129.65Price range: $39.95 through $129.65 -
 Reg´Activ® Essential ME-3$39.95
Reg´Activ® Essential ME-3$39.95
Inflammation
When it comes to heart health, inflammation is a key risk factor. Your gut health can help control inflammation, as is suggested by one small study published in 2012. This study showed that Lactobacillus reuteri could not only reduce LDL cholesterol, but also inflammatory chemicals like C-reactive protein and fibrinogen, making it potentially beneficial for heart health.
Healing After a Heart Attack
Some more recent studies have suggested that microbiota in the gut play a key role in your ability to recover from a heart attack. So far, these studies have only been conducted on mice, but the data so far is promising.
In one of these studies, mice were given antibiotics to kill off gut bacteria a week before being given heart attacks. Various methods were used to reintroduce microbiota into some of the mice, and those mice had better outcomes when it came to immune function and repair after myocardial infarction. Whether probiotics would have the same results for humans remains to be seen, of course.
Questions and Concerns
Naturally, there are a few questions that may arise when looking at this research, including the following:
Can you take probiotics if you have high blood pressure?
The above studies show that probiotics may support healthier blood pressure, so generally yes.
Why do cardiologists warn against probiotics? Can probiotics cause heart problems?
No. Cardiologists’ warnings are typically limited to immunocompromised patients, who may be susceptible to infection.
Improving Your Gut Health
Note that the above studies are all fairly limited with relatively small sample sizes, so more research will be needed to determine the full scope of how probiotics can affect heart health. That said, it does look promising.
In any case, it’s generally beneficial to maintain a healthy balance of gut bacteria. In addition to incorporating fiber and limiting sources of arterial plaque (red meat, poultry, eggs, etc.), probiotics and prebiotics can promote gut health, which may have a positive impact on your heart and other areas.
We suggest that two capsules of Dr. Ohhira’s probiotic supplements per day can supply the prebiotics, and probiotics, and postbiotics needed to maintain a healthy gut. To learn more about the benefits of probiotics, contact us.
References:
i Santiseban MM, et al. Hypertension-linked pathophysiological alterations in the gut. Circ Res. 2017;120:312–323.
ii Kim S, et al. Imbalance of gut microbiome and intestinal epithelial barrier dysfunction in patients with high blood pressure. Clin Sci (Lond). 2018 Mar 30;13(6):701-718.
iii Sun S, et al. The Microbiota Composition and Blood Pressure: The CARDIA Study. Hypertension. 2019 May;73(5):998-1006.
iv Cook R, et al. Lifestyle changes may be more important than drugs for mild hypertension. BMJ. 2019;364:1571.